
Latest News
 Athlete of the Week: Dillan Abbate, Bow High School
Athlete of the Week: Dillan Abbate, Bow High School
 Charlestown plane crash injures one
Charlestown plane crash injures one

One person trapped, killed in Manchester Street fire
One woman died in a fire at an apartment building on Manchester Street in Concord.

Riverbend to close adult mental health housing facility in Concord due to funding challenges
Riverbend Community Mental Health has announced it will close its adult residential home on Fayette Street in Concord this fall, as ongoing state and federal funding shortfalls put pressure on its programs.
Most Read
 One person trapped, killed in Manchester Street fire
One person trapped, killed in Manchester Street fire
 Ayotte vetoes bathroom bill, defeating it for second time in two years
Ayotte vetoes bathroom bill, defeating it for second time in two years
 Concord may finally buy long-closed rail line with hopes of creating city-spanning trail
Concord may finally buy long-closed rail line with hopes of creating city-spanning trail
 Free speech group, residents back Bow parents’ appeal in case involving transgender athletes
Free speech group, residents back Bow parents’ appeal in case involving transgender athletes
 Concord city council divided over raise for city manager to nearly $250K
Concord city council divided over raise for city manager to nearly $250K
 Cannon Mountain tram to shut for at least two years while replacement is installed
Cannon Mountain tram to shut for at least two years while replacement is installed
Editors Picks
 A Webster property was sold for unpaid taxes in 2021. Now, the former owner wants his money back
A Webster property was sold for unpaid taxes in 2021. Now, the former owner wants his money back
 Report to Readers: Your support helps us produce impactful reporting
Report to Readers: Your support helps us produce impactful reporting
 City prepares to clear, clean longstanding encampments in Healy Park
City prepares to clear, clean longstanding encampments in Healy Park
 Productive or poisonous? Yearslong clubhouse fight ends with council approval
Productive or poisonous? Yearslong clubhouse fight ends with council approval
Sports

Concord National LL Softball wins State Championship and moves on to Little League Regional Tournament
The Concord National Youth Softball 12U All-Stars team booked a trip down to Bristol, Conn., to represent New Hampshire in the Little League New England Region Tournament for the second year in a row with a win over Mount Monadnock on Saturday, 13-3.
 Josiah Hakala of Beaver Meadow wins State Amateur golf championship
Josiah Hakala of Beaver Meadow wins State Amateur golf championship
 Athlete of the Week: Grace Saysaw, Concord High School
Athlete of the Week: Grace Saysaw, Concord High School
 Local golfers tee off at 122nd Amateur Championship
Local golfers tee off at 122nd Amateur Championship
Opinion

Opinion: Trumpism in a dying democracy
 Opinion: What Coolidge’s century-old decision can teach us today
Opinion: What Coolidge’s century-old decision can teach us today
 Opinion: The art of diplomacy
Opinion: The art of diplomacy
 Opinion: After Roe: Three years of resistance, care and community
Opinion: After Roe: Three years of resistance, care and community
 Opinion: Iran and Gaza: A U.S. foreign policy of barbarism
Opinion: Iran and Gaza: A U.S. foreign policy of barbarism

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

New Hampshire school phone ban could be among strictest in the country
When Gov. Kelly Ayotte called on the state legislature to pass a school phone ban in January, the pivotal question wasn’t whether the widely popular policy would pass but how far it would go.
 Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump
Arts & Life

Artist Spotlight: Holly Emrick
This week’s artist spotlight, brought to you through a collaboration with the Concord Insider and the Concord Arts Market, focuses on Holly Emrick, who lives in Boscawen. A 58-year-old mother of two and grandmother of two and a wife of 40 years, Emrick discovered jewelry-making during her 16 years as a stay-at-home mom.
 Concert on the lawn coming to Pierce Manse
Concert on the lawn coming to Pierce Manse
 Lavender haze: Purple fields bloom at Warner farm
Lavender haze: Purple fields bloom at Warner farm
 Arts in the Park returns for July
Arts in the Park returns for July
Obituaries
 Lisa M. Hochberg
Lisa M. Hochberg
Concord, NH - Lisa Marie (Huey) Hochberg passed away on Thursday July 10, 2025, in Concord, NH, surrounded by her family. Born on July 9, 1962, in Warren, PA, she was the daughter of John and Patricia (Brothers) Huey. Lisa had very... remainder of obit for Lisa M. Hochberg
 Sue Ann Ross
Sue Ann Ross
Chichester, NH - Sue Ann Ross, 75, of Chichester, passed away at home on July 14, 2025, after a lengthy battle with cancer, surrounded by her loving family. She was born on January 10, 1950, in Concord, NH, to her late parents Earl and ... remainder of obit for Sue Ann Ross
 Sharon Parmenter
Sharon Parmenter
Boscawen , NH - Sharon A. Parmenter, 78, of Boscawen, passed away with family and friends by her bedside on the evening of July 2, 2025 at Concord Hospital. Sharon was born in Plymouth, NH on December 19, 1946, the first daughter to... remainder of obit for Sharon Parmenter
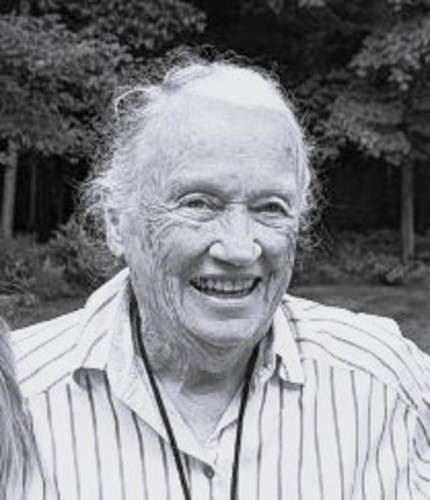 Elizabeth Terrell
Elizabeth Terrell
Concord, NH - Elizabeth "Liz" Terrell passed away on July 12, 2025, at Pine Rock Manor after several months of declining health. She was two months shy of turning 91 years old. She was born on September 15, 1934, in New Rochelle, New Yo... remainder of obit for Elizabeth Terrell

 Universal EFA enrollment set to hit 10,000-student cap
Universal EFA enrollment set to hit 10,000-student cap
 Community Players of Concord celebrate 97th season, prepare for 98th
Community Players of Concord celebrate 97th season, prepare for 98th
 Concord All-Star U-13 Little League baseball to play in East Regional Tournament in Delaware
Concord All-Star U-13 Little League baseball to play in East Regional Tournament in Delaware
 Chichester hires new town administrator after town hall turnover
Chichester hires new town administrator after town hall turnover
 State Sen. Dan Innis launches bid for U.S. Senate, setting primary race with Scott Brown
State Sen. Dan Innis launches bid for U.S. Senate, setting primary race with Scott Brown
 Henniker Blues, Brews & BBQ Fest returns for fourth year
Henniker Blues, Brews & BBQ Fest returns for fourth year

 Youngsters Richardson and Hakala move on, and veterans crash out at 122nd State Amateur Championship
Youngsters Richardson and Hakala move on, and veterans crash out at 122nd State Amateur Championship Concord became a Housing Champion. Now, state lawmakers could eliminate the funding.
Concord became a Housing Champion. Now, state lawmakers could eliminate the funding. ‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference  Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide Nate Lavallee, July Young Professional of the Month: Stretching toward strength, self-care and Southern NH wellness
Nate Lavallee, July Young Professional of the Month: Stretching toward strength, self-care and Southern NH wellness
