Latest News
 Vandals hit mausoleum of Tilton's namesake
Vandals hit mausoleum of Tilton's namesake
 Opinion: Adopting the right 306 Rules
Opinion: Adopting the right 306 Rules

What’s in a name? Ask an Epsom Yeaton.
Norm Yeaton dropped a stack of papers three inches thick, attached by a clip, onto his living room table.The thud said a lot, that an arduous research project by Yeaton – in an attempt to understand the sheer volume of people in Epsom whose last name...

‘We’re just kids’: As lawmakers debate transgender athlete ban, some youth fear a future on the sidelines
Maëlle Jacques has read the articles written about her.“Winner of NH Girls High Jump is Biological Male.”“Transgender girl blasted after dominating New Hampshire girls high jump.”“U.S. ‘Full of Failing Gutless Mothers and Fathers’: High School Boy...
Most Read
Editors Picks
 Concord martial arts studio builds life skills far beyond combat
Concord martial arts studio builds life skills far beyond combat
 Red barn on Warner Road near Concord/Hopkinton line to be preserved
Red barn on Warner Road near Concord/Hopkinton line to be preserved
 FAFSA fiasco hits New Hampshire college goers and universities hard
FAFSA fiasco hits New Hampshire college goers and universities hard
 Searchable Concord salary database: Top earners include more police, fewer women
Searchable Concord salary database: Top earners include more police, fewer women
Sports

Wednesday’s high schools: Fancher’s 2-run blast leads Concord baseball to victory; plus more baseball, softball, lax and tennis results
BaseballConcord 9, Winnacunnet 8Key players: Concord – Matt Jenness (winning pitcher), Jackson Martin (save), Mitch Coffey (3 hits, 2 runs, RBI), Dawson Fancher (2-run HR, 2 hits, 2 runs, 3 RBI), Brett McDonough (2 hits, 2 RBI), Kaelen Williams (hit,...
Opinion

Opinion: Being and becoming: A good doctor in the age of artificial intelligence
Narain Batra, under the auspices of the Osher Institute at Dartmouth, will deliver a public lecture, “Superintelligence: Why We Need It” on May 24. He lives in Hartford, Vermont. A few years ago, I was on a return flight from New Delhi to Paris and...
 Opinion: Bankers have the NH Public Deposit Investment Pool in their sights
Opinion: Bankers have the NH Public Deposit Investment Pool in their sights
 Opinion: Proposed height zoning change for Concord’s Main Street
Opinion: Proposed height zoning change for Concord’s Main Street

Politics

Sununu says he’ll support Trump even if he’s convicted
As jury selection begins this week in the hush-money trial of former President Donald Trump, New Hampshire Gov. Chris Sununu says he doesn’t believe many voters view Trump’s criminal indictments, his actions on Jan. 6, 2021, or his election denialism...
 NH mayors want more help from state on homelessness prevention funds
NH mayors want more help from state on homelessness prevention funds
 Two democrats with parallel views run for same State Senate seat
Two democrats with parallel views run for same State Senate seat
 House passes bill removing exceptions to state voter ID law
House passes bill removing exceptions to state voter ID law
 League of Women Voters suing over AI robocalls sent in NH
League of Women Voters suing over AI robocalls sent in NH
Arts & Life

NH Furniture Masters present new member show this spring
The NH Furniture Masters are pleased to feature the work of three new members in our spring exhibition: Dan Faia, Mike Korsak, and Philip Morley. This exhibit celebrates the creativity and dedication of our newest members and brings together a diverse...
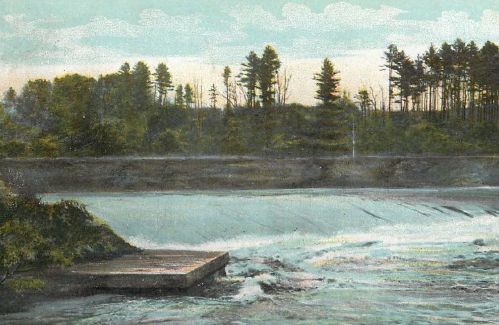 Vintage Views: The greatest factory that never was
Vintage Views: The greatest factory that never was
 Inspired by Robert Frost, New Hampshire Poet Laureate Jennifer Militello has achieved her childhood dreams
Inspired by Robert Frost, New Hampshire Poet Laureate Jennifer Militello has achieved her childhood dreams
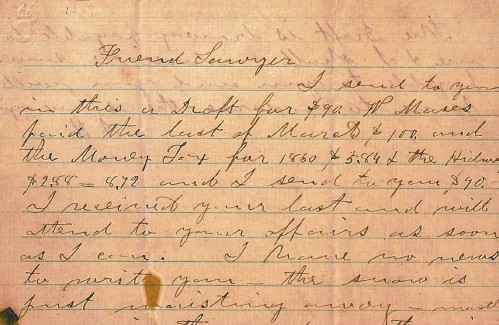 From the archives: Civil War brewing
From the archives: Civil War brewing
Obituaries
 Allen C. Cole
Allen C. Cole
Allan C. Cole Pembroke, NH - Allan C. Cole, 87, of Pembroke, passed away on Wednesday March 27, 2024 at Concord Hospital following a period of declining health. Allan was born on Novembe... remainder of obit for Allen C. Cole
 Kirsten Wirth
Kirsten Wirth
Concord, NH - Kirsten Wirth passed from this life peacefully after a brief battle with cancer, with three of her siblings surrounding her with love at her bedside in Concord, NH on March 29... remainder of obit for Kirsten Wirth
 Cynthia Grudak
Cynthia Grudak
Hayesville, NC - Cynthia Charles Grudak 84, of Murphy, North Carolina passed away Tuesday, April 9, 2024, in a Clay County care facility. She was the daughter of the late Harold and Louise... remainder of obit for Cynthia Grudak
 Kevin Ward Jenkins
Kevin Ward Jenkins
Concord, NH - Kevin Ward Jenkins, 67, died Friday, April 12, 2024 at Concord Hospital, Concord, NH. Born on April 3, 1957 in Concord, NH, Kevin is the son of the late Ward and Charlene ... remainder of obit for Kevin Ward Jenkins

 On the trail: NH GOP leaders urge ‘decorum and respect’
On the trail: NH GOP leaders urge ‘decorum and respect’
 From a book to bread, Merrimack Valley High School students show off their senior projects
From a book to bread, Merrimack Valley High School students show off their senior projects
 Beekeepers, farmers square off in NH Senate committee hearing
Beekeepers, farmers square off in NH Senate committee hearing
 Gallery: Forty-mile gravel bicycle race draws racers from all over the region
Gallery: Forty-mile gravel bicycle race draws racers from all over the region
 The fraught path forward for cannabis legalization, explained
The fraught path forward for cannabis legalization, explained
 Mother of two convicted of negligent homicide in fatal Loudon crash released on parole
Mother of two convicted of negligent homicide in fatal Loudon crash released on parole

 Softball: Maddy Wachter Ks 12, Concord holds off Winnacunnet in 2023 championship rematch
Softball: Maddy Wachter Ks 12, Concord holds off Winnacunnet in 2023 championship rematch High schools: Tuesday’s track, baseball, softball, lacrosse and tennis results
High schools: Tuesday’s track, baseball, softball, lacrosse and tennis results Boys’ lacrosse: With a different level of energy and focus, MV feels primed for success
Boys’ lacrosse: With a different level of energy and focus, MV feels primed for success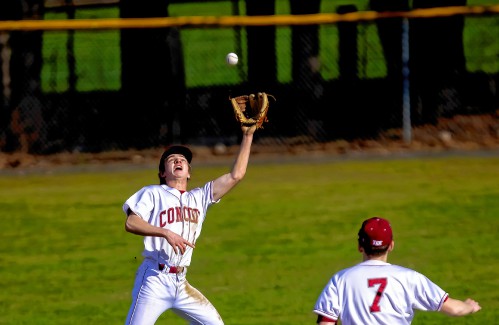 Baseball: Concord makes eight errors but shows reasons for optimism in wild extra-inning loss
Baseball: Concord makes eight errors but shows reasons for optimism in wild extra-inning loss Opinion: Members of NH Jewish community write letter to NH congressional delegation
Opinion: Members of NH Jewish community write letter to NH congressional delegation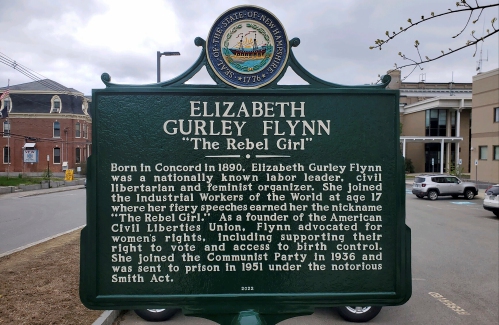 Opinion: Whatever a court decides, Elizabeth Gurley Flynn retains an important place in American labor history
Opinion: Whatever a court decides, Elizabeth Gurley Flynn retains an important place in American labor history Sunapee Kearsarge Intercommunity Theater presents ‘Olympus On My Mind’ in April
Sunapee Kearsarge Intercommunity Theater presents ‘Olympus On My Mind’ in April
