
With new plan for multi-language learners, Concord School District shifts support for New American students
Every time Leanna Kenza laces up her sneakers and steps on the track, it gives her reprieve from the day-to-day drama of eighth grade and the chance to find a new friend.While most Rundlett Middle School parents were enrolling their kids in sports in...

With Concord down to one movie theater, is there a future to cinema-going?
With Concord reduced to a single movie theater for the first time in living memory and New Hampshire chain Chunky’s Cinema Pub closing two of its three locations, going out to the flicks in the Granite State just keeps getting harder.Don’t expect that...
Most Read
 No deal. Laconia buyer misses deadline, state is out $21.5 million.
No deal. Laconia buyer misses deadline, state is out $21.5 million.
 “It’s beautiful” – Eight people experiencing homelessness to move into Pleasant Street apartments
“It’s beautiful” – Eight people experiencing homelessness to move into Pleasant Street apartments
 With Concord down to one movie theater, is there a future to cinema-going?
With Concord down to one movie theater, is there a future to cinema-going?
 Quickly extinguished fire leaves Concord man in critical condition
Quickly extinguished fire leaves Concord man in critical condition
 Concord police ask for help in identifying person of interest in incidents of cars being keyed during Republican Party event
Concord police ask for help in identifying person of interest in incidents of cars being keyed during Republican Party event
Editors Picks
 What’s in a name? Ask an Epsom Yeaton.
What’s in a name? Ask an Epsom Yeaton.
 Downtown cobbler breathes life into tired shoes, the environmentally friendly way
Downtown cobbler breathes life into tired shoes, the environmentally friendly way
 People of color incarcerated at higher rates in New Hampshire, but data is limited
People of color incarcerated at higher rates in New Hampshire, but data is limited
 Former Concord firefighter sues city, claiming years of homophobic sexual harassment, retaliation
Former Concord firefighter sues city, claiming years of homophobic sexual harassment, retaliation
Sports

High schools: Concord girls’ lax picks up first win, Tide softball handed first loss in pitchers’ duel
Girls’ LacrosseConcord 20, Nashua North 7Key players: Concord – Emma Pelletier (8 goals, 5 draw controls), Sofia Payne (6 goals, 2 assist), Sarah Leuci (3 goals, 10 draw controls), Sydney Brown (goal, assist), Ava Philbrook (goal, assist), Malie...
 Patriots’ draft approach likely to be different in post-Belichick era
Patriots’ draft approach likely to be different in post-Belichick era
 High schools: Weekend results
High schools: Weekend results
Opinion

Opinion: The truth of it
John Buttrick writes from his Vermont Folk Rocker in his Concord home, Minds Crossing. He can be reached at johndbuttrick@gmail.com Watching and reading the news today involves frequent exposure to the word “existential,” employed to mean truth....
 Opinion: A bad idea for New Hampshire
Opinion: A bad idea for New Hampshire
 Opinion: Medical Aid in Dying would have spared my father’s suffering
Opinion: Medical Aid in Dying would have spared my father’s suffering
 Opinion: NH youth’s effort for a more robust climate curriculum
Opinion: NH youth’s effort for a more robust climate curriculum
 Opinion: Inherited hatred and how to stop it
Opinion: Inherited hatred and how to stop it

Politics

Charities will not have to pay rent to casinos under new law
Deb Leahy can finally breathe easy, freed from the fluctuating rental fees each time her organization partners with a New Hampshire casino for donations.Thanks to a new law, casinos are now prohibited from imposing rent charges on charities for...
 Sununu says he’ll support Trump even if he’s convicted
Sununu says he’ll support Trump even if he’s convicted
 NH mayors want more help from state on homelessness prevention funds
NH mayors want more help from state on homelessness prevention funds
 Two democrats with parallel views run for same State Senate seat
Two democrats with parallel views run for same State Senate seat
 House passes bill removing exceptions to state voter ID law
House passes bill removing exceptions to state voter ID law
Arts & Life

Celebrate agriculture, education, and community at the NH Farm, Forest, and Garden Expo
Deerfield, NH — The New Hampshire Farm, Forest, and Garden Expo returns this spring, promising an exciting blend of agriculture, education, and family fun.Scheduledfor Friday, May 3, 9 a.m. to 7 p.m. and Saturday, May 4, and 9 a.m. to 4 p.m., the Expo...
 Active Aging: John Burke of Peterborough celebrated his 81st birthday with 81 hikes up Pack Monadnock
Active Aging: John Burke of Peterborough celebrated his 81st birthday with 81 hikes up Pack Monadnock
 Vintage Views: From darkness to light
Vintage Views: From darkness to light
Obituaries
 Joanna M. Cloe
Joanna M. Cloe
formerly of Pembroke, NH - Joanna Mary (Cavanagh) Cloe, 79, passed away in Florida April 17th after a short illness. She was formerly a longtime resident of Pembroke, NH and member of St. John the Baptist Church. She was born in Bat... remainder of obit for Joanna M. Cloe
 Rita A. French
Rita A. French
Contoocook, NH - Rita A. French, age 98, of Park Ave, passed away peacefully on Monday, April 22, 2024 at her home. She was born in Barton, VT one of 7 Children to the late Samuel and Myra (Leonard) Paul. Rita worked at Concord Hos... remainder of obit for Rita A. French
 Elizabeth G. Mahon
Elizabeth G. Mahon
Elizabeth "Betty" G. Mahon Boscawen, NH - Elizabeth "Betty" G. Mahon, age 93, passed away peacefully on Saturday, April 13, 2024 with family by her side. She was born in Salem, MA daughter of the late John and Elizabeth (Tansey) Gannon.... remainder of obit for Elizabeth G. Mahon
 Marylee Meagher
Marylee Meagher
Hudson, NH - Marylee Meagher, 67, of Hudson, passed away Friday, April 19, 2024 at Southern NH Medical Center surrounded by her family and friends. She was born on October 15, 1956 in Nashua, daughter of the late Edgar and Agnes (Le... remainder of obit for Marylee Meagher

 Concord man charged felony criminal mischief following vandalism outside NH GOP event
Concord man charged felony criminal mischief following vandalism outside NH GOP event
 Getaway driver in Winnipesaukee hit-and-run arrested
Getaway driver in Winnipesaukee hit-and-run arrested
 Head of NH Port Authority placed on administrative leave
Head of NH Port Authority placed on administrative leave
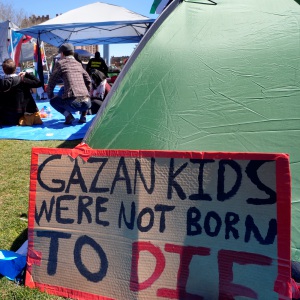 As UNH hosts rally against Gaza war, lawmakers weigh campus free speech protections
As UNH hosts rally against Gaza war, lawmakers weigh campus free speech protections
 Update: Victim identified in Lantern Lane fire in Concord
Update: Victim identified in Lantern Lane fire in Concord
 Opinion: Public school standards overhaul will impact every facet of public education in NH
Opinion: Public school standards overhaul will impact every facet of public education in NH
 High schools: Bow track sweeps 4-team meet at Pembroke
High schools: Bow track sweeps 4-team meet at Pembroke
 Mold found in Bow Community Building
Mold found in Bow Community Building

 High schools: Coe-Brown softball wins 5th straight, Concord’s McDonald pitches first varsity win, Tide’s Doherty scores 100th career point
High schools: Coe-Brown softball wins 5th straight, Concord’s McDonald pitches first varsity win, Tide’s Doherty scores 100th career point High schools: Bow’s Kelly lifts Falcon softball to victory in walk-off, more Monday results, plus Saturday’s track meets
High schools: Bow’s Kelly lifts Falcon softball to victory in walk-off, more Monday results, plus Saturday’s track meets Community Players of Concord present newest adaptation of Pride and Prejudice
Community Players of Concord present newest adaptation of Pride and Prejudice Concord Monitor editor Mike Pride’s final book explores the lives, works of Northern New England poets
Concord Monitor editor Mike Pride’s final book explores the lives, works of Northern New England poets
