Latest News

Regal Theater in Concord is closing Thursday
After Thursday’s 7:30 p.m. showing of “Kung Fu Panda 4,” the Regal Cinema on Loudon Road will close for good, ending 28 years of multiplex movies on The Heights in Concord and marking the latest step in the redevelopment of the Steeplegate Mall.What’s...

With less than three months left, Concord Casino hasn’t found a buyer
At the start of the year, Concord Casino was ordered to close its doors and sell the business within six months, but, so far, no buyers have stepped forward to acquire the establishment.“There’s been no change in the status of the Concord facility,”...
Most Read
Editors Picks
 Concord martial arts studio builds life skills far beyond combat
Concord martial arts studio builds life skills far beyond combat
 Red barn on Warner Road near Concord/Hopkinton line to be preserved
Red barn on Warner Road near Concord/Hopkinton line to be preserved
 Hometown Hero: Quilters, sewers grateful for couple continuing ‘treasured’ business
Hometown Hero: Quilters, sewers grateful for couple continuing ‘treasured’ business
 Searchable Concord salary database: Top earners include more police, fewer women
Searchable Concord salary database: Top earners include more police, fewer women
Sports

Obiri, Lemma claim Boston Marathon
BOSTON — Sisay Lemma of Ethiopia set a blistering pace and held on to win the Boston Marathon on Monday, running alone through most of the course to finish in 2 hours, 6 minutes, 17 seconds — the 10th-fastest time in the race’s 128-year history.Hellen...
 High schools: Concord boys’ lax earns first win, plus more weekend results
High schools: Concord boys’ lax earns first win, plus more weekend results
 High schools: Wednesday and Thursday’s results
High schools: Wednesday and Thursday’s results
 Bow girls’ lacrosse coach Chris Raabe achieves milestone win
Bow girls’ lacrosse coach Chris Raabe achieves milestone win
 High schools: Bow girls’ lax coach Raabe wins 300th game, more Wednesday results
High schools: Bow girls’ lax coach Raabe wins 300th game, more Wednesday results
Opinion

Opinion: Members of NH Jewish community write letter to NH congressional delegation
Bob Sanders lives in Concord. On a rainy April 10, I with the help of one other delivered a message on behalf of 67 New Hampshire Jews to the office of Rep. Annie Kuster in Concord, calling for a ceasefire in Gaza, humanitarian aid, and cutting off...
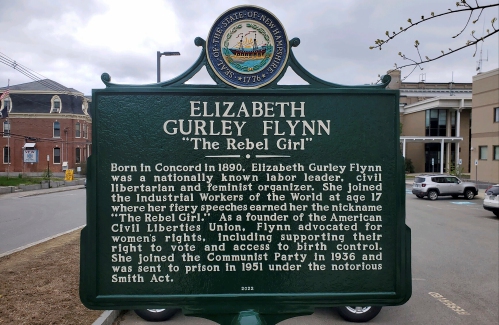 Opinion: Whatever a court decides, Elizabeth Gurley Flynn retains an important place in American labor history
Opinion: Whatever a court decides, Elizabeth Gurley Flynn retains an important place in American labor history
 Opinion: How our twin toddlers turned our lives (and chairs) upside down
Opinion: How our twin toddlers turned our lives (and chairs) upside down
 Opinion: New Hampshire, it’s time to drive into the future
Opinion: New Hampshire, it’s time to drive into the future
 Opinion: Eid al-Fitr in Gaza: A war against humanity itself
Opinion: Eid al-Fitr in Gaza: A war against humanity itself

Politics

Two democrats with parallel views run for same State Senate seat
Angela Brennan of Bow and Rebecca McWilliams of Concord, both Democratic State Representatives, have entered the race for the New Hampshire State Senate in District 15, to fill the shoes of Sen. Becky Whitley, who is eyeing a congressional seat.The...
 House passes bill removing exceptions to state voter ID law
House passes bill removing exceptions to state voter ID law
 League of Women Voters suing over AI robocalls sent in NH
League of Women Voters suing over AI robocalls sent in NH
 As NH lawmakers eye statewide housing solutions, local control remains a barrier
As NH lawmakers eye statewide housing solutions, local control remains a barrier
 On the trail: Haley was first in and last out
On the trail: Haley was first in and last out
Arts & Life
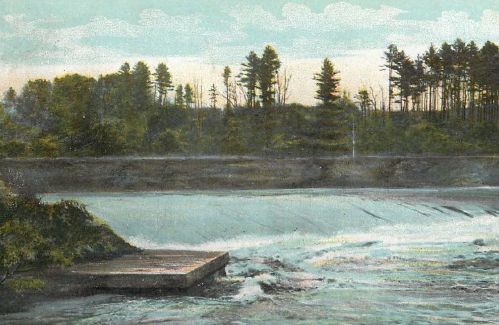
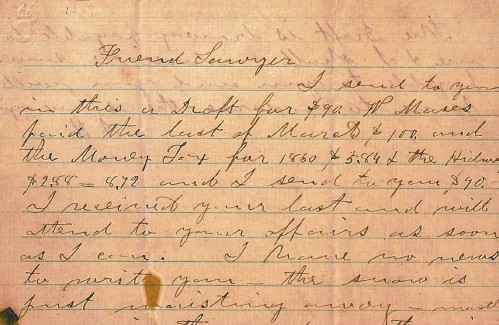
Vintage Views: The greatest factory that never was
It was almost two hundred years ago when our Concord ancestors thought and planned and then they planned and thought again. They dreamed about what could be and about the riches that might follow. A period of time commonly referred to as the Second...
 Inspired by Robert Frost, New Hampshire Poet Laureate Jennifer Militello has achieved her childhood dreams
Inspired by Robert Frost, New Hampshire Poet Laureate Jennifer Militello has achieved her childhood dreams
 From the archives: Civil War brewing
From the archives: Civil War brewing
 From the farm: Celebrate springtime
From the farm: Celebrate springtime
 National Water Dances comes to NH
National Water Dances comes to NH
Obituaries
 Jane A. Haskell
Jane A. Haskell
Boscawen , NH - Jane A. Haskell, 95, died peacefully on Saturday April 13, 2024, at Merrimack County Nursing Home. She was born in Dover, NH, the daughter of Amy (Towle) and Harold Brow... remainder of obit for Jane A. Haskell
 Patricia L. Hews
Patricia L. Hews
Concord, NH - Patricia L. Hews passed away peacefully on April 3, 2024. "Pat," as she was known by most, was born on November 30, 1931 in Dover-Foxcroft, Maine. She is the daughter to Marga... remainder of obit for Patricia L. Hews
 Candice Myatt
Candice Myatt
Rochester, NH - Candice E Myatt, 74 of Rochester NH, formerly of Barnstead NH passed away unexpectedly on Wednesday evening at her home. She grew up in Weare NH with her father Carl Hoyt Sr... remainder of obit for Candice Myatt
 Darla Jean Welcome
Darla Jean Welcome
Penacook, NH - Darla Jean Welcome died very unexpectantly on Friday April 7, 2024. Darla was predeceased by her husband Dean Welcome and father David Randlett Jr. She is survived by her mot... remainder of obit for Darla Jean Welcome

 High schools: Tuesday’s track, baseball, softball, lacrosse and tennis results
High schools: Tuesday’s track, baseball, softball, lacrosse and tennis results
 Boys’ lacrosse: With a different level of energy and focus, MV feels primed for success
Boys’ lacrosse: With a different level of energy and focus, MV feels primed for success
 Concord city-schools committee revived, will meet for first time in 2 years
Concord city-schools committee revived, will meet for first time in 2 years
 Phenix Hall, Christ the King food pantry, rail trail on Concord planning board’s agenda
Phenix Hall, Christ the King food pantry, rail trail on Concord planning board’s agenda
 Sununu says he’ll support Trump even if he’s convicted
Sununu says he’ll support Trump even if he’s convicted
 NH mayors want more help from state on homelessness prevention funds
NH mayors want more help from state on homelessness prevention funds
 Opinion: Proposed height zoning change for Concord’s Main Street
Opinion: Proposed height zoning change for Concord’s Main Street
 Baseball: Concord makes eight errors but shows reasons for optimism in wild extra-inning loss
Baseball: Concord makes eight errors but shows reasons for optimism in wild extra-inning loss
 High schools: Monday’s baseball, softball, lacrosse and tennis results
High schools: Monday’s baseball, softball, lacrosse and tennis results


