Newly retired state medical examiner reflects on 20-year career
| Published: 09-18-2017 12:41 AM |
In his 20 years as New Hampshire’s medical examiner, Dr. Thomas Andrew has consulted with medical specialists, weapons specialists, crime-scene specialists, specialists about which bugs get attracted to corpses – and, once, a plant specialist.
“It involved an 18-year-old guy, a landscaper, who had pulled up a plant and showed it to his brother and said ‘Hey, look at this, a wild parsnip like mom makes in soup!’ He takes a bite out of it and in 45 minutes he’s dead,” recalled Andrew, who has just retired after two decades in charge of the medical agency that examines all “sudden, unexpected or unnatural” deaths within New Hampshire.
“So I’m trying to identify the plant with books. I decide what I think it is and send a picture to a botanist at UNH,” Andrew said. “I got an email back saying, ‘You’re a moron! Haven’t you seen this before?’ It was pokeweed.”
UNH didn’t really call Andrew a moron – he was spicing up the story a bit – but he was quick to defend himself by noting that having grown up in Ohio, he isn’t familiar with our weed makeup. “Pokeweed kills a lot of pigs every year; if you’re a pig farmer, you know pokeweed. It has a digitalis-like substance in the root. But without the botanist, I would have not known what to test for, where to go with this,” he said.
And that, says Andrew, who practiced as a pediatrician before switching to forensic medicine, is an illustration of what makes being a medical examiner so interesting.
“It clearly is the practice of medicine – plus more,” he said.
As a practicing physician, “for a complex problem, you’re going to consult with another physician. Not so in forensic medicine – complex problems might be tackled by different specialists that have nothing to do with medicine. You talk to a tool-mark analyst, a hair and fiber expert, somebody who’s skilled in blood-spatter analysis, a forensic anthropologist for skeletal remains.
“The scope of inquiry is so much broader.”
Article continues after...
Yesterday's Most Read Articles
Being a medical examiner, a doctor whose patients are always dead, is an unusual specialty for a physician, admits Andrew, 61. It’s also one that colleagues tend to look down on.
“Many (medical) residents don’t dare to whisper their interest in the field. Academics are shocked, they’re so disappointed: ‘Why would you want to waste all this excellent training in pulling bullets?’ ” he said. “Anybody who thinks a forensic pathologist is a hunchbacked Quasimodo in the basement with no social interaction has the wrong image.”
This is true even though forensic medicine has become “sexy” due to its depiction on police and medical shows.
At conferences, Andrew said, colleagues “love to talk about it. They say ‘tell me about it, tell me stories.’ But I think it’s more to a curiosity akin to a layperson’s curiosity, than any professional curiosity.”
“This comes off like I’m whining,” he added. “I’m not, but I don’t think the specialty is held in high regard by academics, even by clinicians.”
One result, Andrew said, is that it can be difficult to hire medical examiners. That’s an issue because the state office workload has exploded as the opioid crisis has swept into New Hampshire.
Andrew says the workload forced him to drop a long-standing policy of performing an autopsy on every suspected drug death in the state. He and Dr. Jennie Duval, the assistant medical examiner who is replacing Andrew in the office, will do about 500 autopsies this year. He said the office currently only autopsies obvious drug-overdose deaths when questions arise or law enforcement needs evidence.
The Legislature has approved a third medical examiner, but for the time being stand-ins will be hired.
The lack of medical respect for forensic autopsies reflects a general trend about all autopsies. For reasons that are much debated, the number of autopsies performed in this county has been falling for decades: In 1972, according to the Centers for Disease Control, 19.3 percent of all deaths – not just suspicious deaths – were given an autopsy. By 2007, that figure had fallen more than half, to 8.5 percent.
“There are many reasons. Fear of the medical legal system, liability, and some of it is professional hubris. Clinicians with all of their whizbang tech and radiographic studies say that (autopsy) is an archaic, 18th-century procedure that can’t tell us anything,” Andrew said. “New construction hospitals in the United States don’t even build an autopsy room!”
“Yet study after study after study shows that the autopsy serves a valuable quality assurance and quality control function,” he said.
As an example, he pointed to a basic medical question: What is the normal weight for the heart of a healthy person? That’s an important data point when assessing hypertension cardiovasulcar disease or judging the effect of drug usage.
“We are basing our assessments of normal heart weight on charts that were generated in the 1920s and ’30s. Nobody will do that study anymore because there aren’t enough hearts to weigh – because people won’t get autopsies!” he said. “Jennie and I are hard-pressed to go into the files and find a significant percentage of people with ‘normal’ hearts. Everybody has a big heart! What has changed? We don’t know … and nobody can do the study.”
In fact, autopsies are getting so uncommon that it affects medical education.
“Even Dartmouth-Hitchcock Medical Center, an academic teaching hospital, is having trouble getting their pathology residents enough autopsies to sit for the boards,” Andrew said.
Dr. Andrew got his medical license at the University of Cincinnati and practiced pediatrics at Cincinnati Children’s Hospital, but says he became intrigued with forensics in medical school and eventually did a second residency in the field. In 1991, he was hired by the New York City medical examiner’s office.
“It was training by immersion,” he said. “The year I got there was the first year that they topped 2,000 homicides in a year.” In contrast, all of New Hampshire recorded 16 homicides last year.
As might be expected, there’s a certain reputation attached to working in New York. “You walk out of there with a lot of swagger: I’m New York trained!” Andrew said.
But when a third child arrived, Andrew and his wife, Rebecca, a psychiatrist, began thinking of settling down in a quieter environment. That’s when he heard that the position in New Hampshire was open following the untimely death at age 46 of Dr. Roger Fossum, who had virtually created the medical examiner position in the late 1980s.
He got the job and the family, now in Hopkinton, moved to New Hampshire. Andrew says he quickly found that big-city training can leave gaps.
“I thought I’d seen everything. Then you come to New Hampshire, and you’re: ‘Long guns? What are long guns?’ Or ‘It’s a logging accident? Are you kidding me?’ ” he recalled.
As a branch of law enforcement – state law says the office’s role is to “investigate medico-legal cases” – the medical examiner’s office is part of many high-profile cases, including suspect deaths in police custody, major homicides, and deaths of prominent people. Controversy can be part of the job and it’s not unknown for medical examiners to be sued by family members who are unhappy with the ruling of a cause of death, usually because it involved suicide or illegal substances.
“There’s a website out there that has me as Satan incarnate because of the way I handled their loved one’s death,” said Andrew.
Over the years, the office has published several times in the Morbidity and Mortality Weekly Report, a digest compiled by the Centers for Disease Control that is distributed nationally, including an early report on a death from Lyme disease, as well as early insight into the “choking game” in which people deliberately cut off their oxygen supply to feel a natural euphoria. The game has led to hundreds of deaths, mostly among children and teens, and Andrew has lectured about it throughout the country and overseas.
And despite what we’ve all seen on TV shows, Andrew says medical examiners are not Sherlock Holmes in a medical gown.
“There have been a couple of instances where we have aided (police) significantly, putting them on a path perhaps different than they started on,” he said. “But the ‘Aha!’ thing at an autopsy, where you solve (a case), is fiction.”
And speaking of fiction, what does Andrew think of his profession’s depiction in film and television? Not surprisingly, not much.
“I don’t watch them,” he said. “Whatever little snippets I have seen of fictional (medical forensics) is so fictional as to not to be fun to watch.”
In particular, the ability to determine time of death is not what mysteries have led us to believe: “It is almost always a range and the range is much broader than the public, and certainly prosecutors, would like. Very often that range isn’t much different from the last time they were seen alive and when they were found dead.”
“I’m sure it’s fun if you don’t have a sense of what it’s really like. I can watch a legal drama and have fun because I don’t know squat about being a lawyer,” he added.
In New Hampshire, autopsies are generally performed in a special room in the basement of Concord Hospital, not far from the medical examiner’s office. It is basically a standard operating room with one big difference: “It’s not sterile. I don’t have to be concerned about infecting the patient,” said Andrew. It’s also somewhat cooler than operating rooms, to help preserve the body.
Obviously, Andrew has a different interaction with patients than he did as a pediatrician (where, he noted dryly, “I loved the kids – the parents, not so much.”).
“The big adjustment is in the examining room. It’s much more like a surgeon’s professional relationship with their patient; very measured, scientific, controlled. The place where I practice my bedside manner, so to speak, is in the phone calls with the families, next of kin. We’ll say this is what we saw, what we think is going on, this is where the case is headed, or this is the cause of death, this is why your loved one died,” he said.
The cause of death in cases that come to the medical examiner are often fairly obvious, but not always.
“If I find two or three things at autopsy that have lethal potential, I have to correlate my findings with that person’s history, with what the scene and circumstances tell us about the final hours or minutes, and other material, and that might point to one of those causes being most likely,” he said.
And what about the psychological cost of being a physician who can never save their patient?
“This is an odd niche, and the coping skills that are necessary sometimes may be different,” said Andrew.
The key is to realize that the medical examiner’s patient isn’t really the body on the operating table – it’s also the family, the community, even the concept of justice.
“I am their advocate, their only advocate from a medical standpoint, but it’s not being done for them,” he said.
But it can be hard, he said, recalling a triple homicide involving a young mother and two toddlers.
“The major crime unit had responded to it hours before. They were doing the macho thing around the crime van, having coffee, talking. I came and did my thing, and I was strutting around, too,” Andrew recalled.
But then, he said, the prosecutor walked to the back of the house “and caught me back there, crying. … It was an important lesson; if you don’t allow yourself to be moved, if you detach all your humanity, you’d better get out.”
And when you’re off work, “You’d better have something other than drugs or alcohol – whether it’s a great support system at home, a faith tradition that you honor and respect, or something else.”
He points to a second home in Randolph: “How healing and refreshing that is, to be in the North Country, up on a ledge somewhere, looking down on peaceful, sun-dappled autumn leaves. If you don’t have something like that, if you go home to a bottle or pills or something, you’re in trouble.”
Dr. Andrew isn’t totally leaving medical forensics. He will continue his work with White Mountain Forensic Consulting, in which he consults about medical forensic findings, and often testifies in court, for cases outside New Hampshire, usually on behalf of defendants.
He is also lugging around a quarter-century of paperwork on all his autopsies, including those in New York, because there’s no statute of limitations for civil lawsuits that might be brought for accidental deaths.
In fact, he said, on the day he retired he was deposed – questioned as part of a lawsuit – about findings from an autopsy he performed clear back in 1993. “They were surprised I still had the paperwork,” he recalled.
The other major part of his post-medical examiner life will be studying at the United Theological Seminary in Dayton, Ohio.
His goal is to become chaplain for the Daniel Webster Council of Boy Scouts, which covers all of New Hampshire. Andrew and his family have been involved with the Boy Scouts for many years, and has found that his profession carries a certain weight among the young-male crowd.
“Oh yeah – you get a cachet,” he said. He plans to coordinate a “CSI-type activity” at the annual Jamboree event.
As for why Andrew is retiring now, he says he announced years ago that he would do it at this time, after putting in 20 years on the job. “Twenty years is kind of the point where things can get stale,” he said. “I don’t want that to happen.”
(David Brooks can be reached at 369-3313 or dbrooks@cmonitor.com or on Twitter @GraniteGeek.)


 With less than three months left, Concord Casino hasn’t found a buyer
With less than three months left, Concord Casino hasn’t found a buyer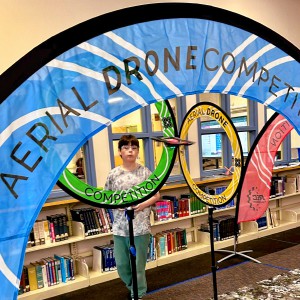 Kearsarge Middle School drone team headed to West Virginia competition
Kearsarge Middle School drone team headed to West Virginia competition Phenix Hall, Christ the King food pantry, rail trail on Concord planning board’s agenda
Phenix Hall, Christ the King food pantry, rail trail on Concord planning board’s agenda Granite Geek: Forest streams are so pretty; too bad they’re such a pain to measure
Granite Geek: Forest streams are so pretty; too bad they’re such a pain to measure
