
Latest News
 Treetop Gem: The Brilliant Blackburnian Warbler
Treetop Gem: The Brilliant Blackburnian Warbler
 Vintage Views: The ugliest dog wins
Vintage Views: The ugliest dog wins
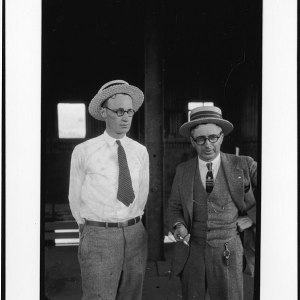 Opinion: Monkey Trial centennial
Opinion: Monkey Trial centennial

Hometown Hero: Franklin’s Kandyce Mohan
From working in the drug prevention field to now administering government funds for prevention efforts across the state, Kandyce Mohan’s event planning and organizational skills first sprouted in Franklin.

‘Life long friends’: Three women worked together to welcome visitors to East Concord
After almost a decade of work by three women to rally support and raise funds for a marker showcasing the East Concord Gardening Club, the granite sign is up and welcoming drivers to the historic area.
Most Read
Editors Picks
 A Webster property was sold for unpaid taxes in 2021. Now, the former owner wants his money back
A Webster property was sold for unpaid taxes in 2021. Now, the former owner wants his money back
 Report to Readers: Your support helps us produce impactful reporting
Report to Readers: Your support helps us produce impactful reporting
 City prepares to clear, clean longstanding encampments in Healy Park
City prepares to clear, clean longstanding encampments in Healy Park
 Productive or poisonous? Yearslong clubhouse fight ends with council approval
Productive or poisonous? Yearslong clubhouse fight ends with council approval
Sports

Sunapee’s Bryce Whitlow keeps memory of above-average MLB players alive through social media page ‘MLB Hall of (Pretty) Good’
Bryce Whitlow has worked as a paraeducator in Sunapee for two years, but outside of his day job, he’s the man behind a social media page called “MLB Hall of (Pretty) Good” that has taken online baseball media by storm.
 Concord Monitor Spring Players of the Season
Concord Monitor Spring Players of the Season
Opinion

Opinion: What Coolidge’s century-old decision can teach us today
One hundred years ago this July, a quiet man from Vermont — Calvin Coolidge — made a decision that changed the course of Sino-American relations.
 Opinion: The art of diplomacy
Opinion: The art of diplomacy
 Opinion: After Roe: Three years of resistance, care and community
Opinion: After Roe: Three years of resistance, care and community
 Opinion: Iran and Gaza: A U.S. foreign policy of barbarism
Opinion: Iran and Gaza: A U.S. foreign policy of barbarism
 Opinion: There’s no place like firearms-free zones
Opinion: There’s no place like firearms-free zones

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

New Hampshire school phone ban could be among strictest in the country
When Gov. Kelly Ayotte called on the state legislature to pass a school phone ban in January, the pivotal question wasn’t whether the widely popular policy would pass but how far it would go.
 Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump
Arts & Life

AROUND CONCORD: Your guide to free summer music
With a good camp chair, a cool beverage and a worn, cozy sweatshirt, the perfect New England summer evening might just be enjoying the music of local musicians at dusk.
 Around Concord: Steps to nowhere – but it used to be somewhere
Around Concord: Steps to nowhere – but it used to be somewhere
 Around Concord: Refreshing recipes from Table Bakery
Around Concord: Refreshing recipes from Table Bakery
 The Rebel Collective to perform in Henniker
The Rebel Collective to perform in Henniker
 Meet Moriah Billups, Young Professional of the Year
Meet Moriah Billups, Young Professional of the Year
Obituaries
 Warren Steele
Warren Steele
George Warren Steele, friend of theater, ballet dancer on the tennis court, died December 16, 2024 in the good hands of the Ascension Medical Center, Austin Texas. He spent his final days discussing atheism and theology with his nurses, and ... remainder of obit for Warren Steele
 Rodolphe Arthur Begin
Rodolphe Arthur Begin
Rodolphe "Rudy" Arthur Begin Concord, NH - Rodolphe "Rudy" Arthur Begin, age 94, of Concord passed away on Sunday, June 29, 2025 at Presidential Oaks in Concord. He was born the son of the late Joseph and Nora (LeCompte) Begin. He was a... remainder of obit for Rodolphe Arthur Begin
 Joseph Michael Morrison
Joseph Michael Morrison
Concord, NH - Joseph Michael Morrison, age 54, of Fairview Drive, passed away on Tuesday, July 1st, 2025 at Brigham and Women's Hospital in Boston surrounded by his family and friends after a long battle with cancer. Joe was born in... remainder of obit for Joseph Michael Morrison
 Norman Jackson Robinson
Norman Jackson Robinson
Billerica, MA - Norman Jackson Robinson, 86, an extraordinarily kind and generous man, passed away peacefully at his home surrounded by his loving family. Norman was born September 23, 1938, at the United Fruit Company Hospital in Tela,... remainder of obit for Norman Jackson Robinson

 New Hampshire home prices hit an all-time record high amid housing shortage
New Hampshire home prices hit an all-time record high amid housing shortage
 Opinion: The ink is dry on the state budget, and Republicans’ priorities are clear
Opinion: The ink is dry on the state budget, and Republicans’ priorities are clear
 As Concord’s Gavin Richardson places second at golf Junior Amateur, young players look ahead to the 122nd State Amateur Championship
As Concord’s Gavin Richardson places second at golf Junior Amateur, young players look ahead to the 122nd State Amateur Championship
 Warner shot down a housing developer’s bid. New statewide zoning mandates could clear a path for proposals like it.
Warner shot down a housing developer’s bid. New statewide zoning mandates could clear a path for proposals like it.

 Six local seniors play in CHaD East-West All-Star Football game; Nyhan wins MVP
Six local seniors play in CHaD East-West All-Star Football game; Nyhan wins MVP Athlete of the Week: Nate Kiah, Bow Falcons
Athlete of the Week: Nate Kiah, Bow Falcons Track & field: Hopkinton’s Lane wins New England title in 3,200 meters, Concord’s Saysaw runs state record times in 100 and 200
Track & field: Hopkinton’s Lane wins New England title in 3,200 meters, Concord’s Saysaw runs state record times in 100 and 200 Concord became a Housing Champion. Now, state lawmakers could eliminate the funding.
Concord became a Housing Champion. Now, state lawmakers could eliminate the funding. ‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference  Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide
