
‘Something to chase’: Pascal Zabayo’s art fundraiser grows soccer from Concord to Kampala, Uganda
Pascal Zabayo chased his biggest dreams when he moved to New Hampshire in 2016.

‘It’s a ritual’: Best practices and benefits in caring for bonsai
When Isabel Burley first delved into the world of bonsai a few years ago, she discovered a plethora of possibilities for growing plants.
Most Read
 ‘Would you raise your right hand?’ — Local veterans consider the meaning of Memorial Day
‘Would you raise your right hand?’ — Local veterans consider the meaning of Memorial Day
 New Hampshire school phone ban could be among strictest in the country
New Hampshire school phone ban could be among strictest in the country
 Jesse Sullivan pleads guilty to second-degree murder of half-brother, Zackary
Jesse Sullivan pleads guilty to second-degree murder of half-brother, Zackary
 Loudon police received a mental health call. Here’s how they avoided escalating it.
Loudon police received a mental health call. Here’s how they avoided escalating it.
 Photos: Memorial Day parade in Concord
Photos: Memorial Day parade in Concord
 Opinion: Hopkinton students speak out on youth sports and poverty
Opinion: Hopkinton students speak out on youth sports and poverty
Editors Picks
 The Monitor’s guide to the New Hampshire legislature
The Monitor’s guide to the New Hampshire legislature
 One year after UNH protest, new police body camera footage casts doubt on assault charges against students
One year after UNH protest, new police body camera footage casts doubt on assault charges against students
 ‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
 ‘We honor your death’ – Arranging services for those who die while homeless in Concord
‘We honor your death’ – Arranging services for those who die while homeless in Concord
Sports

Track & field: Belmont’s Lacasse, Takantjas win four events each to lead Red Raiders to Wilderness League Championship title
With one week to go until the NHIAA track and field division championships, the Belmont girls’ team showed its a favorite for the crown by winning the 23-team Wilderness League Championship at Newfound Regional High School on Saturday.
Opinion

Opinion: How dark can it get?
Jonathan P. Baird lives in Wilmot.
 Opinion: Unfair taxes, unfair schools: The New Hampshire way
Opinion: Unfair taxes, unfair schools: The New Hampshire way
 Opinion: In the fight to stop sexual violence, can polio hold the solutions?
Opinion: In the fight to stop sexual violence, can polio hold the solutions?
 Opinion: Where are the permanent solutions for a more stable budget?
Opinion: Where are the permanent solutions for a more stable budget?
 Opinion: My memories of Vietnam 50 years later
Opinion: My memories of Vietnam 50 years later

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

New Hampshire school phone ban could be among strictest in the country
When Gov. Kelly Ayotte called on the state legislature to pass a school phone ban in January, the pivotal question wasn’t whether the widely popular policy would pass but how far it would go.
 Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump
Arts & Life

Artist Spotlight: Brittany Batchelder
With creativity abounding in the community around us, The Concord Insider, in collaboration with Concord Arts Market, highlights local artists on a regular basis.
 Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
 Beautify Allenstown hosting community cleanup day
Beautify Allenstown hosting community cleanup day
Obituaries
 Richard E. Phelps
Richard E. Phelps
Richard "Dick" E. Phelps Epsom, NH - Richard "Dick" E. Phelps, 90, beloved husband, father, grandfather, uncle and friend, transitioned from this life on Saturday, May 17, 2025. Dick was born on May 16, 1935, in Rutland, VT, the son of ... remainder of obit for Richard E. Phelps
 Bruce Bouldry
Bruce Bouldry
Concord, NH - Bruce Hamilton Bouldry -- August 14 1961 - January 17, 2025 Bruce Bouldry passed peacefully at Concord Hospital surrounded by his loving family after a brief period of illness. Bruce was born and raised in Brockton, Ma... remainder of obit for Bruce Bouldry
 Gerard Armand Cote
Gerard Armand Cote
Concord, NH - Gerard (Jerry) Armand Cote, Sr., 85, passed away May 21, 2025, at Granite VNA Hospice House, after a brief illness. He was born in Dover, NH on July 5, 1939, to Armand and Antoinette Cote (Gosselin). As a young man, he wor... remainder of obit for Gerard Armand Cote
 Brenda Melendy
Brenda Melendy
Warner, NH - Brenda R. Melendy, beloved wife, mother, grandmother, and friend, passed away peacefully at home on May 21, 2025, with family at her side. Born on February 17, 1941, in Jamaica Plain, MA, Brenda grew up on the West Side of ... remainder of obit for Brenda Melendy

 There has been rain on two-thirds of the days in May, and more on the way
There has been rain on two-thirds of the days in May, and more on the way
 Boys’ Lacrosse: Bean reaches milestone in Coe-Brown win over BowBears eat Falcons in heavy hitters matchup, 13-3
Boys’ Lacrosse: Bean reaches milestone in Coe-Brown win over BowBears eat Falcons in heavy hitters matchup, 13-3
 High schools: Hillsboro-Deering sweeps Hopkinton; Tuesday’s baseball, softball, lacrosse and tournament tennis
High schools: Hillsboro-Deering sweeps Hopkinton; Tuesday’s baseball, softball, lacrosse and tournament tennis
 Athlete of the Week: Emma Pelletier, Concord High School
Athlete of the Week: Emma Pelletier, Concord High School
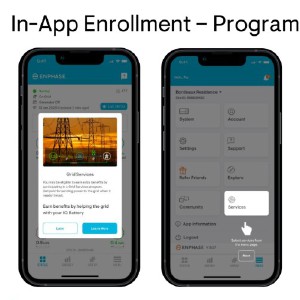 Granite Geek: Take advantage of living on the edge of the grid
Granite Geek: Take advantage of living on the edge of the grid
 High schools: Concord softball falls on Senior Day; Stark, Brady baseball win on Memorial Day
High schools: Concord softball falls on Senior Day; Stark, Brady baseball win on Memorial Day
 Immigration and the arts council: What to look for in the State House this week
Immigration and the arts council: What to look for in the State House this week

 High schools: Final regular season track and tennis results; plus weekend baseball, softball and lacrosse
High schools: Final regular season track and tennis results; plus weekend baseball, softball and lacrosse Girls’ lacrosse: Bow bounces back with 13-3 win over Bishop Brady
Girls’ lacrosse: Bow bounces back with 13-3 win over Bishop Brady High schools: John Stark’s Philibotte pitches shutout, hits game-winning RBI in 1-0 win, plus more results from Wednesday
High schools: John Stark’s Philibotte pitches shutout, hits game-winning RBI in 1-0 win, plus more results from Wednesday High schools: Freitas 1-hitter leads Hopkinton softball to shutout; Tuesday’s baseball, lax, tennis and track results
High schools: Freitas 1-hitter leads Hopkinton softball to shutout; Tuesday’s baseball, lax, tennis and track results Concord became a Housing Champion. Now, state lawmakers could eliminate the funding.
Concord became a Housing Champion. Now, state lawmakers could eliminate the funding. ‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference  Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide Young Professional of the Month Katie Duncan shares about creativity, community, connection
Young Professional of the Month Katie Duncan shares about creativity, community, connection Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
