
‘Insult to injury’ – Military honors and burial denied for mother in Pembroke murder-suicide
In a quiet corner of Blossom Hill Cemetery, two modest grave markers stand side by side on a bare patch of earth where fresh grass is just beginning to grow—Julia Byrne, 26, on the left, and her three-year-old son, Blake, on the right.

‘Shining our light as bright as the sun’ – Merrimack Valley graduates urged to care for others
Jacqueline Pearl is in love with her future and can’t wait to meet her.
Most Read
Editors Picks
 Missing in Manchester: A timeline of the missing persons investigation for Glenn Chrzan
Missing in Manchester: A timeline of the missing persons investigation for Glenn Chrzan
 Inside EFAs: How school vouchers have fueled a Christian school enrollment boom in New Hampshire
Inside EFAs: How school vouchers have fueled a Christian school enrollment boom in New Hampshire
 ‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
 ‘We honor your death’ – Arranging services for those who die while homeless in Concord
‘We honor your death’ – Arranging services for those who die while homeless in Concord
Sports

High schools: Bow, Hopkinton girls’ lax advance to D-III semis; baseball prelims
No. 5 Bow 16, No. 4 John Stark 8
 Girls’ lacrosse: Second half comeback sends MV to semis
Girls’ lacrosse: Second half comeback sends MV to semis
Opinion

Opinion: Concord should be run like a household, not a business
This My Turn was originally presented as testimony at a city council hearing.
 Opinion: Our leaders’ puzzling decision to eliminate the State Council on the Arts
Opinion: Our leaders’ puzzling decision to eliminate the State Council on the Arts
 Opinion: How dark can it get?
Opinion: How dark can it get?
 Opinion: Unfair taxes, unfair schools: The New Hampshire way
Opinion: Unfair taxes, unfair schools: The New Hampshire way
 Opinion: In the fight to stop sexual violence, can polio hold the solutions?
Opinion: In the fight to stop sexual violence, can polio hold the solutions?

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

New Hampshire school phone ban could be among strictest in the country
When Gov. Kelly Ayotte called on the state legislature to pass a school phone ban in January, the pivotal question wasn’t whether the widely popular policy would pass but how far it would go.
 Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump
Arts & Life

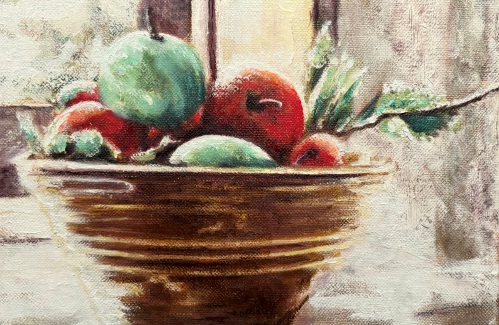
White Mountain art exhibition makes new home at New Hampshire Historical Society
The New Hampshire Historical Society’s newest exhibition, “A Legacy of Landscapes: Selections from the Linda and P. Andrews McLane Collection,” displays more than 60 paintings of White Mountain landscape art from a single private collection. Most of these paintings have not been on view to the public for many years.
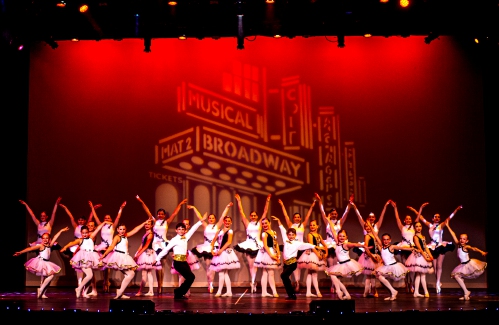
 A sneak peak of summer events in the Concord area
A sneak peak of summer events in the Concord area
 Pierce Manse reopens for the season
Pierce Manse reopens for the season
 Vintage Views: The Liars Club
Vintage Views: The Liars Club
 Two Villages Art Society begins summer members show
Two Villages Art Society begins summer members show
Obituaries
 Maureen A. Anderson
Maureen A. Anderson
Maureen A Anderson Framingham, MA - Maureen Anderson, 84, formerly of Manchester and Concord, passed away May, 27, with her family by her side. Maureen was a sociable, funny and lovely woman with a taste for beauty. She was also a lovin... remainder of obit for Maureen A. Anderson
 Charles Willis Brown Jr.
Charles Willis Brown Jr.
Charles Willis Brown Jr Weare, NH - Charles W. Brown Jr, 91, of Weare, passed away peacefully at his home in Weare on May 15, 2025. Born in Concord, NH, on September 8, 1933, the fourth child of Charles Sr. and Barbara (Eddy) Brown. His ... remainder of obit for Charles Willis Brown Jr.
 Michael Vanaskie
Michael Vanaskie
Tampa, FL - Dr. Michael J. Vanaskie, PhD, beloved husband, father, and grandfather, passed away on May 26, 2025, at the age of 78. Born in Shamokin, Pennsylvania, Michael devoted his life to the well-being of others, leaving a legacy of... remainder of obit for Michael Vanaskie
 Paul Trombly
Paul Trombly
Paul (Bunk) Trombly Loudon, NH - Passed away on May 31, 2025. He was born on March 9, 1934 in Concord, NH, to Napoleon and Gertrude (Foley) Trombly. He is survived by his loving wife, Roberta (O'Keefe) Trombly; his children, Paula Burr,... remainder of obit for Paul Trombly


 High schools: John Stark baseball advances to final four, Franklin softball falls in quarters
High schools: John Stark baseball advances to final four, Franklin softball falls in quarters
 Girls’ lacrosse: Bow falls to top-seeded St. Thomas in semis, 17-6
Girls’ lacrosse: Bow falls to top-seeded St. Thomas in semis, 17-6
 Girls’ lacrosse: Hopkinton falls to Gilford in, 18-2, in rainy semifinal
Girls’ lacrosse: Hopkinton falls to Gilford in, 18-2, in rainy semifinal
 Vintage Views: The Concord Mayoral Race Fiasco of 1939
Vintage Views: The Concord Mayoral Race Fiasco of 1939
 ‘Brady being Brady’: Graduating seniors reflect on lessons learned at Bishop Brady High School
‘Brady being Brady’: Graduating seniors reflect on lessons learned at Bishop Brady High School
 Hopkinton graduates leaned on each other to get through high school
Hopkinton graduates leaned on each other to get through high school
 Licensed Nursing Assistant program for New Americans sends off first graduates
Licensed Nursing Assistant program for New Americans sends off first graduates
 Homeyer: Gardening in difficult conditions
Homeyer: Gardening in difficult conditions

 Baseball: John Stark’s Philibotte named D-II Player of the Year, All-State teams released
Baseball: John Stark’s Philibotte named D-II Player of the Year, All-State teams released High schools: Softball prelims and other spring tournament results
High schools: Softball prelims and other spring tournament results Boys’ tennis: Kearsarge claims third D-III title in five years, Bishop Brady makes first appearance since 1973
Boys’ tennis: Kearsarge claims third D-III title in five years, Bishop Brady makes first appearance since 1973 Concord became a Housing Champion. Now, state lawmakers could eliminate the funding.
Concord became a Housing Champion. Now, state lawmakers could eliminate the funding. ‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference  Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide
