
Owners of Lewis Farm prepare to bring back agritourism after long dispute with city of Concord
The surviving remnants of a commercial kitchen collect dust in the back room of James Meinecke’s farm stand.

‘Folks who use it should pay for it’ — City manager proposes clubhouse plan with smaller tax impact
When City Manager Tom Aspell introduced a new, scaled-back design for a rebuilt clubhouse at the Beaver Meadow Golf Course on Thursday, he concluded by agreeing with a common refrain from the project’s critics.
Most Read
 ‘I thought we had some more time’ – Coping with the murder-suicide of a young Pembroke mother and son
‘I thought we had some more time’ – Coping with the murder-suicide of a young Pembroke mother and son
 The Appalachian Trail in New Hampshire just got easier, as another debate looms over replacing structures in wilderness areas
The Appalachian Trail in New Hampshire just got easier, as another debate looms over replacing structures in wilderness areas
 Senate stalls bill that would’ve eliminated annual car inspections in New Hampshire
Senate stalls bill that would’ve eliminated annual car inspections in New Hampshire
 Two Weare select board members resign
Two Weare select board members resign
 ‘We need all of you’ – New Hampshire lacks more foster families. Local recruitment efforts are trying to change that
‘We need all of you’ – New Hampshire lacks more foster families. Local recruitment efforts are trying to change that
 Owners of Lewis Farm prepare to bring back agritourism after long dispute with city of Concord
Owners of Lewis Farm prepare to bring back agritourism after long dispute with city of Concord
Editors Picks
 The Monitor’s guide to the New Hampshire legislature
The Monitor’s guide to the New Hampshire legislature
 One year after UNH protest, new police body camera footage casts doubt on assault charges against students
One year after UNH protest, new police body camera footage casts doubt on assault charges against students
 ‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
 ‘We honor your death’ – Arranging services for those who die while homeless in Concord
‘We honor your death’ – Arranging services for those who die while homeless in Concord
Sports

High schools: Wednesday’s baseball, softball, lacrosse, tennis and track results
Bow 12, Kennett 0, 5 inn.
 High schools: Tuesday’s baseball, softball, lax, tennis and track results
High schools: Tuesday’s baseball, softball, lax, tennis and track results
 Baseball: Syvertson suits up for CCA in narrow win over Franklin
Baseball: Syvertson suits up for CCA in narrow win over Franklin
 High schools: Monday’s softball, baseball, lax, tennis and track results
High schools: Monday’s softball, baseball, lax, tennis and track results
 High schools: Weekend lacrosse results
High schools: Weekend lacrosse results
Opinion

Opinion: Where are the permanent solutions for a more stable budget?
Scott Metzger lives in Hopkinton.
 Opinion: My memories of Vietnam 50 years later
Opinion: My memories of Vietnam 50 years later
 Opinion: Concord officials: Can we sit and talk?
Opinion: Concord officials: Can we sit and talk?
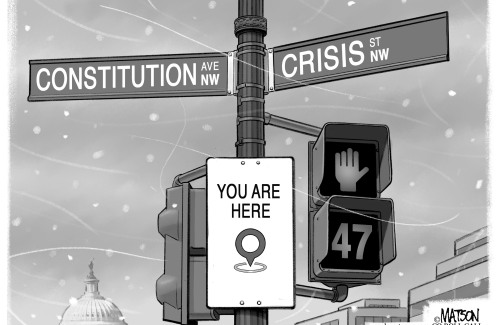 Opinion: Trump versus the U.S. Constitution
Opinion: Trump versus the U.S. Constitution
 Opinion: Protect our winters!
Opinion: Protect our winters!

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
Rosemarie Rung thinks of Elijah Lewis often.
 Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump
Arts & Life

Young Professional of the Month Katie Duncan shares about creativity, community, connection
Meet Katie Duncan, Membership Manager and Educational Outreach Coordinator at the Capitol Center for the Arts. The 35-year old Concord resident’s passion for the arts and the Concord community shines through her work. From theater stages to local lakes, Katie shares how growing up in Greater Concord shaped her path—and why she’s dedicated to giving back.
 Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
 Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
 Beautify Allenstown hosting community cleanup day
Beautify Allenstown hosting community cleanup day
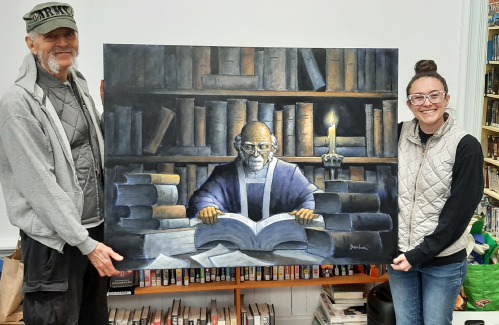 Donating “The Bibliophile”
Donating “The Bibliophile”
Obituaries
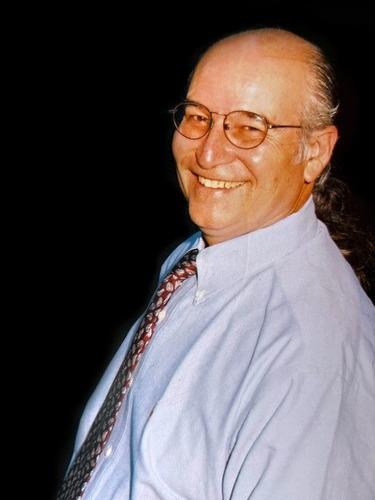
 Gary Clayton Bedell
Gary Clayton Bedell
Pittsburg, NH - Gary Clayton Bedell, 88, of Pittsburg, NH, passed away peacefully on April 29, 2025, after a lengthy illness, surrounded by his loving family. Born on November 27, 1936, in Lancaster, NH he was the son of the late Cl... remainder of obit for Gary Clayton Bedell
 Frederick T. Ford
Frederick T. Ford
Tilton, NH - Frederick "Fred" T. Ford, 87 of Tilton, NH, passed away on Thursday, May 8, 2025, surrounded by his loving family. Born on June 10, 1937, in Jersey City, New Jersey, to the late Frederick V. and Margaret (McNally) Ford. He ... remainder of obit for Frederick T. Ford
 Todd Alan Miller
Todd Alan Miller
Penacook, NH - Todd Alan Miller, 61, passed away peacefully at home on April 26th, 2025. He was the beloved son of Donald and Joyce Miller, and a devoted father, grandfather, brother, and friend. Todd graduated from Merrimack Valley Hi... remainder of obit for Todd Alan Miller
 Joseph Kimball LaBonte
Joseph Kimball LaBonte
Loudon, NH - It is with heavy hearts that we announce the passing of our brother Joseph Kimball LaBonte, 76, on 1/25/25 at Central Valley Medical Center, Nephi, Utah, after a short period of failing health. He was born 12/2/1948 in Con... remainder of obit for Joseph Kimball LaBonte

 Vintage Views: Our very old graves
Vintage Views: Our very old graves
 Opinion: In the fight to stop sexual violence, can polio hold the solutions?
Opinion: In the fight to stop sexual violence, can polio hold the solutions?
 ‘Like going back in time’: Old homes, a train, and a temple added to state historic register
‘Like going back in time’: Old homes, a train, and a temple added to state historic register
 Who would invest in movie theaters these days? These folks
Who would invest in movie theaters these days? These folks
 Boys’ tennis: Growing the sport, fun and pizza for a tight-knit Concord team on Senior Night
Boys’ tennis: Growing the sport, fun and pizza for a tight-knit Concord team on Senior Night
 Concord stargazer puzzled over unidentified flying object
Concord stargazer puzzled over unidentified flying object
 ‘Let them guide us’: New Hampshire honors 55 officers who died in the line of duty
‘Let them guide us’: New Hampshire honors 55 officers who died in the line of duty
 High schools: Concord girls win elite Merrimack Invitational, MV track sweeps senior day, Winnisquam’s Caruso wins 175th career victory, more results from Thursday
High schools: Concord girls win elite Merrimack Invitational, MV track sweeps senior day, Winnisquam’s Caruso wins 175th career victory, more results from Thursday

 Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide Medical aid in dying, education funding, transgender issues: What to look for in the State House this week
Medical aid in dying, education funding, transgender issues: What to look for in the State House this week On the Trail: Shaheen’s retirement sparks a competitive NH Senate race
On the Trail: Shaheen’s retirement sparks a competitive NH Senate race
