
‘Perfect fit’: Fabulous Looks Boutique shifts leadership, preserving brands and styles
Fabulous Looks has been a home away from home for owner Sherry Spurr for over 30 years.

Granite Geek: As quantum mechanics turns 100, it is sneaking into everyday life
There is no science more removed from practical life than quantum mechanics. Or so I thought.
Most Read
 Concord may finally buy long-closed rail line with hopes of creating city-spanning trail
Concord may finally buy long-closed rail line with hopes of creating city-spanning trail
 New Hampshire targets sexual exploitation and human trafficking inside massage parlors
New Hampshire targets sexual exploitation and human trafficking inside massage parlors
 State rules Epsom must pay open-enrollment tuition to other school districts, despite its refraining from the program
State rules Epsom must pay open-enrollment tuition to other school districts, despite its refraining from the program
 New Cheers owners honor restaurant’s original menu while building something fresh
New Cheers owners honor restaurant’s original menu while building something fresh
 Remembered: Friends recall stories about the lives of those who died without housing
Remembered: Friends recall stories about the lives of those who died without housing
 A look ahead at the ‘preferred design’ for Concord’s new police headquarters
A look ahead at the ‘preferred design’ for Concord’s new police headquarters
Editors Picks
 A Webster property was sold for unpaid taxes in 2021. Now, the former owner wants his money back
A Webster property was sold for unpaid taxes in 2021. Now, the former owner wants his money back
 Report to Readers: Your support helps us produce impactful reporting
Report to Readers: Your support helps us produce impactful reporting
 City prepares to clear, clean longstanding encampments in Healy Park
City prepares to clear, clean longstanding encampments in Healy Park
 Productive or poisonous? Yearslong clubhouse fight ends with council approval
Productive or poisonous? Yearslong clubhouse fight ends with council approval
Sports

Youngsters Richardson and Hakala move on, and veterans crash out at 122nd State Amateur Championship
ROCHESTER — Every golfer has A routine. Superstitions, lucky charms and a specific way of finding a mental sweet spot aren’t specific to the sport.
 Athlete of the Week: Grace Saysaw, Concord High School
Athlete of the Week: Grace Saysaw, Concord High School
 Local golfers tee off at 122nd Amateur Championship
Local golfers tee off at 122nd Amateur Championship
Opinion

Opinion: Trumpism in a dying democracy
 Opinion: What Coolidge’s century-old decision can teach us today
Opinion: What Coolidge’s century-old decision can teach us today
 Opinion: The art of diplomacy
Opinion: The art of diplomacy
 Opinion: After Roe: Three years of resistance, care and community
Opinion: After Roe: Three years of resistance, care and community
 Opinion: Iran and Gaza: A U.S. foreign policy of barbarism
Opinion: Iran and Gaza: A U.S. foreign policy of barbarism

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

New Hampshire school phone ban could be among strictest in the country
When Gov. Kelly Ayotte called on the state legislature to pass a school phone ban in January, the pivotal question wasn’t whether the widely popular policy would pass but how far it would go.
 Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump
Arts & Life

Lavender haze: Purple fields bloom at Warner farm
The lavender fields at Pumpkin Blossom Farm in Warner are open for Harvest Days.
 Arts in the Park returns for July
Arts in the Park returns for July
 Hopkinton art gallery showcases “Creativity Beyond Convention”
Hopkinton art gallery showcases “Creativity Beyond Convention”
 AROUND CONCORD: Your guide to free summer music
AROUND CONCORD: Your guide to free summer music
 Around Concord: Steps to nowhere – but it used to be somewhere
Around Concord: Steps to nowhere – but it used to be somewhere
Obituaries
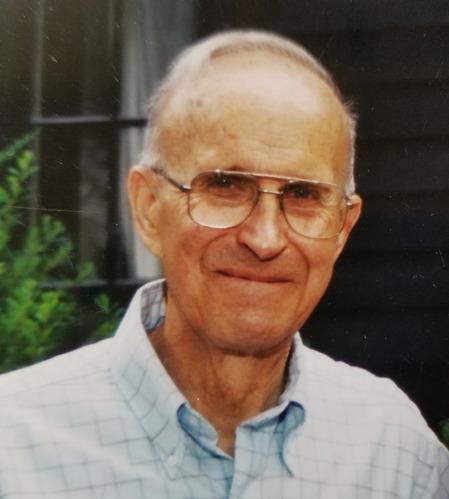
 John W. Herbert
John W. Herbert
Salisbury, NH - John W. Herbert, a proud Navy veteran, devoted family man, and longtime member of the Salisbury community, passed away peacefully on June 28, 2025, at the age of 82. Born and raised in City Island in the Bronx, New York... remainder of obit for John W. Herbert
 Sharon Sargent
Sharon Sargent
Concord, NH - Sharon Mitchell Sargent of 33 Christian Avenue in Concord passed away on July 11, 2025 following a brief illness. Born on October 18, 1944 in Lynn, MA, Sharon, a long-time resident of Gilford, NH was the daughter of Paul ... remainder of obit for Sharon Sargent
 Herbert Little
Herbert Little
Concord, NH - Herbert E. "Herb" Little died on the evening of July 6, 2025, at Havenwood Heritage Heights in the room he shared with his loving wife Debby who was, as always, by his side. He was 97 years old having been born on Septembe... remainder of obit for Herbert Little
 Anna Marie O'Reilly
Anna Marie O'Reilly
Contoocook, NH - Anna Marie O'Reilly, 21, of Contoocook, passed away unexpectedly at home on Friday, July 4, 2025. She was born on June 10, 2004, in Concord, NH to her parents, Joseph P. O'Reilly and Donna M. (Phillips) O'Reilly. Anna g... remainder of obit for Anna Marie O'Reilly


 Free speech group, residents back Bow parents’ free speech appeal in case involving transgender athletes
Free speech group, residents back Bow parents’ free speech appeal in case involving transgender athletes
 Opinion: What does redemption really mean?
Opinion: What does redemption really mean?
 ZBA appointment to be reconsidered at Monday Council meeting
ZBA appointment to be reconsidered at Monday Council meeting
 Opinion: As people of faith, the state budget offends our values
Opinion: As people of faith, the state budget offends our values
 Summer baseball peaks as Concord faces Weare in American Legion play
Summer baseball peaks as Concord faces Weare in American Legion play

 As Concord’s Gavin Richardson places second at golf Junior Amateur, young players look ahead to the 122nd State Amateur Championship
As Concord’s Gavin Richardson places second at golf Junior Amateur, young players look ahead to the 122nd State Amateur Championship Sunapee’s Bryce Whitlow keeps memory of above-average MLB players alive through social media page ‘MLB Hall of (Pretty) Good’
Sunapee’s Bryce Whitlow keeps memory of above-average MLB players alive through social media page ‘MLB Hall of (Pretty) Good’ Concord became a Housing Champion. Now, state lawmakers could eliminate the funding.
Concord became a Housing Champion. Now, state lawmakers could eliminate the funding. ‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference  Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide
