Latest News
 Vintage Views: The Great Cattle Roundup of 1947
Vintage Views: The Great Cattle Roundup of 1947
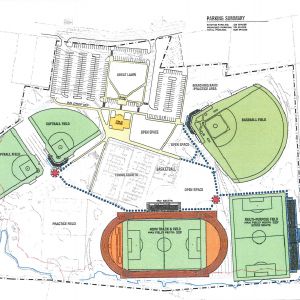 Plans advance on $27M Memorial Field project
Plans advance on $27M Memorial Field project
 Artist Spotlight: Brittany Batchelder
Artist Spotlight: Brittany Batchelder
 Fire at Bradford house kills four pets
Fire at Bradford house kills four pets

Giving life back to board sports: Back Alley Boards upcycles boards into art
Snowboarding, skateboarding and surfing are great ways to stay active, but once a board gets scraped and beat up, most people move on from their well-loved piece of equipment and store it in the garage or toss it away. Back Alley Boards, the brainchild of three New Hampshire artists, gives these boards new life by upcycling and turning them into art.

Memorial Day events in the Concord area
Memorial Day provides a time for solemn remembrance of those who died serving their country. Many local towns hold ceremonies or events to commemorate these lives lost in service. Here is a list of local Memorial Day events.
Most Read
 By all appearances, Canadians are leery of coming to NH
By all appearances, Canadians are leery of coming to NH
 Helen Hanks resigns as Department of Corrections commissioner
Helen Hanks resigns as Department of Corrections commissioner
 “A dream come true” – Family opens housing for adults with disabilities in Concord
“A dream come true” – Family opens housing for adults with disabilities in Concord
 N.H. Senate passes bathroom bill, sending it to Ayotte’s desk
N.H. Senate passes bathroom bill, sending it to Ayotte’s desk
 Catherine Masterson named next superintendent of Merrimack Valley and Andover starting in 2026
Catherine Masterson named next superintendent of Merrimack Valley and Andover starting in 2026
 ‘You made a difference’ — Belmont baseball seniors honor their educators
‘You made a difference’ — Belmont baseball seniors honor their educators
Editors Picks
 The Monitor’s guide to the New Hampshire legislature
The Monitor’s guide to the New Hampshire legislature
 One year after UNH protest, new police body camera footage casts doubt on assault charges against students
One year after UNH protest, new police body camera footage casts doubt on assault charges against students
 ‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
 ‘We honor your death’ – Arranging services for those who die while homeless in Concord
‘We honor your death’ – Arranging services for those who die while homeless in Concord
Sports

Girls’ lacrosse: Bow bounces back with 13-3 win over Bishop Brady
Bow needed to bounce back after their five-game win streak was cut short but John Stark on Monday. Josie Johnson swooped in with a first-half hat-trick alongside a strong Falcons front line to win easily at home and keep moving toward the playoffs.
Opinion

Opinion: Unfair taxes, unfair schools: The New Hampshire way
Ted Morgan is a retired professor of political science living in Tamworth.
 Opinion: In the fight to stop sexual violence, can polio hold the solutions?
Opinion: In the fight to stop sexual violence, can polio hold the solutions?
 Opinion: Where are the permanent solutions for a more stable budget?
Opinion: Where are the permanent solutions for a more stable budget?
 Opinion: My memories of Vietnam 50 years later
Opinion: My memories of Vietnam 50 years later
 Opinion: Concord officials: Can we sit and talk?
Opinion: Concord officials: Can we sit and talk?

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

Concord became a Housing Champion. Now, state lawmakers could eliminate the funding.
In December, Concord’s work to clear the path for more housing hit a new level.
Arts & Life

Young Professional of the Month Katie Duncan shares about creativity, community, connection
Meet Katie Duncan, Membership Manager and Educational Outreach Coordinator at the Capitol Center for the Arts. The 35-year old Concord resident’s passion for the arts and the Concord community shines through her work. From theater stages to local lakes, Katie shares how growing up in Greater Concord shaped her path—and why she’s dedicated to giving back.
 Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
 Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
 Beautify Allenstown hosting community cleanup day
Beautify Allenstown hosting community cleanup day
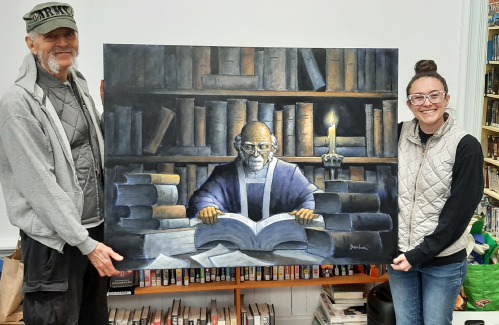 Donating “The Bibliophile”
Donating “The Bibliophile”
Obituaries
 Doris M. McCormack
Doris M. McCormack
Doris M. "Dot" McCormack Barnstead, NH - Doris M. "Dot" McCormack, 81, of Barnstead, NH, passed away peacefully on May 16, 2025, after a brief illness. She was born on April 9, 1944, in New Bedford, MA, daughter of the late Lucien and L... remainder of obit for Doris M. McCormack
 Cynthia Atwell
Cynthia Atwell
Cynthia "Cindi" Atwell Barnstead, NH - Cynthia "Cindi" Atwell, 73, of Barnstead, NH, passed away peacefully on May 13, 2025, surrounded by her loving family after a long and courageous battle with dementia and cancer. Born on December 1... remainder of obit for Cynthia Atwell
 Roger Lincoln Sullivan
Roger Lincoln Sullivan
New London, NH - Roger Lincoln Sullivan, 85, of Clover Lane, died Sunday, May 18, 2025 at his home. He was born in Bridgeport, CT on February 12, 1940 the son of Albert L. and Edith (Riley) Sullivan. Roger was raised in Stratford, ... remainder of obit for Roger Lincoln Sullivan
 James Richard Mikesell
James Richard Mikesell
James "Jim" Richard Mikesell Concord, NH - James Richard Mikesell, 82, a resident of Concord, NH, passed away on May 9, 2025, surrounded by his loving family. He was born on May 30, 1942, to his late parents, Reuben Byron and Mary Ellen ... remainder of obit for James Richard Mikesell

 Drought is completely gone from New Hampshire – maybe it can stop raining now?
Drought is completely gone from New Hampshire – maybe it can stop raining now?
 Concord businesses receive grants to build self-sufficiency
Concord businesses receive grants to build self-sufficiency
 N.E. will have enough electricity this summer but future winters may start to get dicey
N.E. will have enough electricity this summer but future winters may start to get dicey

 High schools: John Stark’s Philibotte pitches shutout, hits game-winning RBI in 1-0 win, plus more results from Wednesday
High schools: John Stark’s Philibotte pitches shutout, hits game-winning RBI in 1-0 win, plus more results from Wednesday High schools: Freitas 1-hitter leads Hopkinton softball to shutout; Tuesday’s baseball, lax, tennis and track results
High schools: Freitas 1-hitter leads Hopkinton softball to shutout; Tuesday’s baseball, lax, tennis and track results High schools: Belmont’s Divers pitches perfect game; Monday’s baseball, softball, lacrosse and tennis results
High schools: Belmont’s Divers pitches perfect game; Monday’s baseball, softball, lacrosse and tennis results High schools: Pelletier scores 100th goal, leads Concord girls’ lax to first win; baseball, softball, boys’ lacrosse and track results from this weekend
High schools: Pelletier scores 100th goal, leads Concord girls’ lax to first win; baseball, softball, boys’ lacrosse and track results from this weekend ‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference  Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide Medical aid in dying, education funding, transgender issues: What to look for in the State House this week
Medical aid in dying, education funding, transgender issues: What to look for in the State House this week
