Latest News
 Athlete of the Week: Jaden Haas
Athlete of the Week: Jaden Haas

‘Friends of the Beav’ want people to see the city’s golf course differently
The friends of Beaver Meadow Golf Course and its harshest critics can agree on one thing: In most places, golf is a sport that keeps its door shut to many people.

“A dream come true” – Family opens housing for adults with disabilities in Concord
The credit should go to Liam Dennehy, at least that’s what his parents think.
Most Read
 Helen Hanks resigns as Department of Corrections commissioner
Helen Hanks resigns as Department of Corrections commissioner
 As Canadian travel to the U.S. falls, North Country businesses are eyeing this Victoria Day weekend to predict impacts in New Hampshire
As Canadian travel to the U.S. falls, North Country businesses are eyeing this Victoria Day weekend to predict impacts in New Hampshire
 ‘I thought we had some more time’ – Coping with the murder-suicide of a young Pembroke mother and son
‘I thought we had some more time’ – Coping with the murder-suicide of a young Pembroke mother and son
 Owners of Lewis Farm prepare to bring back agritourism after long dispute with city of Concord
Owners of Lewis Farm prepare to bring back agritourism after long dispute with city of Concord
 ‘It's how we fight back’: Youth demonstrate at “No Voice Too Small” rally
‘It's how we fight back’: Youth demonstrate at “No Voice Too Small” rally
Editors Picks
 The Monitor’s guide to the New Hampshire legislature
The Monitor’s guide to the New Hampshire legislature
 One year after UNH protest, new police body camera footage casts doubt on assault charges against students
One year after UNH protest, new police body camera footage casts doubt on assault charges against students
 ‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
‘It’s always there’: 50 years after Vietnam War’s end, a Concord veteran recalls his work to honor those who fought
 ‘We honor your death’ – Arranging services for those who die while homeless in Concord
‘We honor your death’ – Arranging services for those who die while homeless in Concord
Sports

High schools: Pelletier scores 100th goal, leads Concord girls’ lax to first win; baseball, softball, boys’ lacrosse and track results from this weekend
Concord 14, Nashua North 9
Opinion

Opinion: In the fight to stop sexual violence, can polio hold the solutions?
Molly McHugh is the Director of Communications at No Means No Worldwide, an organization dedicated to ending sexual violence. She lives in Orford.
 Opinion: Where are the permanent solutions for a more stable budget?
Opinion: Where are the permanent solutions for a more stable budget?
 Opinion: My memories of Vietnam 50 years later
Opinion: My memories of Vietnam 50 years later
 Opinion: Concord officials: Can we sit and talk?
Opinion: Concord officials: Can we sit and talk?
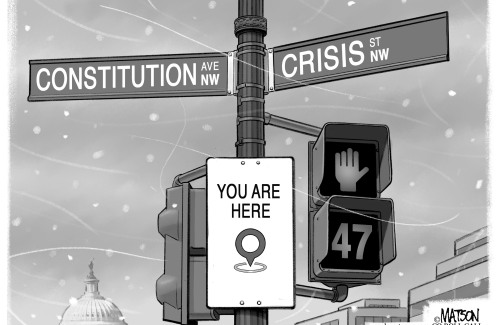 Opinion: Trump versus the U.S. Constitution
Opinion: Trump versus the U.S. Constitution

Your Daily Puzzles

An approachable redesign to a classic. Explore our "hints."

A quick daily flip. Finally, someone cracked the code on digital jigsaw puzzles.

Chess but with chaos: Every day is a unique, wacky board.

Word search but as a strategy game. Clearing the board feels really good.

Align the letters in just the right way to spell a word. And then more words.
Politics

‘A wild accusation’: House votes to nix Child Advocate after Rep. suggests legislative interference
Rosemarie Rung thinks of Elijah Lewis often.
 Sununu decides he won’t run for Senate despite praise from Trump
Sununu decides he won’t run for Senate despite praise from Trump
Arts & Life

Young Professional of the Month Katie Duncan shares about creativity, community, connection
Meet Katie Duncan, Membership Manager and Educational Outreach Coordinator at the Capitol Center for the Arts. The 35-year old Concord resident’s passion for the arts and the Concord community shines through her work. From theater stages to local lakes, Katie shares how growing up in Greater Concord shaped her path—and why she’s dedicated to giving back.
 Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
Tiny Tapestry sale at Red River Theaters raising money for Concord Coalition to End Homelessness
 Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
Bowling for a cause: Angelman Syndrome Fundraiser coming to Boutwell’s
 Beautify Allenstown hosting community cleanup day
Beautify Allenstown hosting community cleanup day
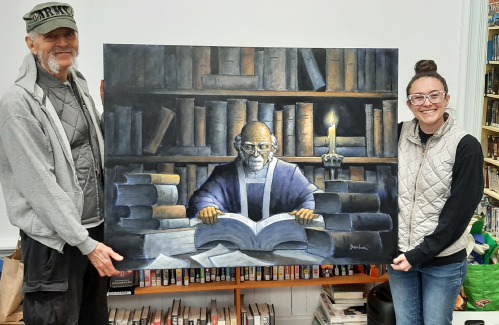 Donating “The Bibliophile”
Donating “The Bibliophile”
Obituaries
 Timothy Harkness
Timothy Harkness
Lakeland, FL - Tim Harkness, age 61, of Lakeland, FL passed away peacefully on April 30, 2025. He was born on July 30, 1963 in Vermont and grew up in Epsom, NH. He had moved to Florida in 2018. He had always loved cars and had multiple ... remainder of obit for Timothy Harkness
 Cody Chamberlain
Cody Chamberlain
Franklin, NH - It is with great sadness that we announce the unexpected passing of Cody James Chamberlain on May 17, 2025, at the age of 28 due to a motorcycle accident. Cody was born on July 29, 1996, and was the beloved son of Win... remainder of obit for Cody Chamberlain
 Alan Kanegsberg
Alan Kanegsberg
Dedham, MA - Alan Kanegsberg (March 6, 1940) passed away peacefully at 85 (May 17, 2025). Alan leaves his devoted wife of 63 years, Helaine (Rosenberg), sons Howard and Philip, beloved grandson Torston, and sister Samantha K. Burkey. Al... remainder of obit for Alan Kanegsberg
 Phyllis R. Kelley
Phyllis R. Kelley
Gilmanton, NH - Phyllis R. Kelley fondly called Dolly by family and friends died May 4, 2025 just one day shy of her 101 Birthday, at Golden View Health Care Center, Meredith, NH following a brief illness. Phyllis was born in Pittsf... remainder of obit for Phyllis R. Kelley

 Remembering Sarah Kinter, descendant of Nathaniel Peabody Rodgers, “Friend of the Slave”
Remembering Sarah Kinter, descendant of Nathaniel Peabody Rodgers, “Friend of the Slave”
 High schools: Freitas 1-hitter leads Hopkinton softball to shutout; Tuesday’s baseball, lax, tennis and track results
High schools: Freitas 1-hitter leads Hopkinton softball to shutout; Tuesday’s baseball, lax, tennis and track results
 Bakery in New Hampshire wins in free speech case over a pastry shop painting
Bakery in New Hampshire wins in free speech case over a pastry shop painting
 Boys’ Lacrosse: Falcons fire away and shut down Laconia in the second half to win, 11-2
Boys’ Lacrosse: Falcons fire away and shut down Laconia in the second half to win, 11-2
 High schools: Belmont’s Divers pitches perfect game; Monday’s baseball, softball, lacrosse and tennis results
High schools: Belmont’s Divers pitches perfect game; Monday’s baseball, softball, lacrosse and tennis results

 Five former Concord Crush girls at St. Paul’s are soon to leave the nest to play NCAA Women’s Lacrosse
Five former Concord Crush girls at St. Paul’s are soon to leave the nest to play NCAA Women’s Lacrosse Boys’ tennis: Growing the sport, fun and pizza for a tight-knit Concord team on Senior Night
Boys’ tennis: Growing the sport, fun and pizza for a tight-knit Concord team on Senior Night High schools: Concord girls win elite Merrimack Invitational, MV track sweeps senior day, Winnisquam’s Caruso wins 175th career victory, more results from Thursday
High schools: Concord girls win elite Merrimack Invitational, MV track sweeps senior day, Winnisquam’s Caruso wins 175th career victory, more results from Thursday High schools: Wednesday’s baseball, softball, lacrosse, tennis and track results
High schools: Wednesday’s baseball, softball, lacrosse, tennis and track results Town elections offer preview of citizenship voting rules being considered nationwide
Town elections offer preview of citizenship voting rules being considered nationwide Medical aid in dying, education funding, transgender issues: What to look for in the State House this week
Medical aid in dying, education funding, transgender issues: What to look for in the State House this week On the Trail: Shaheen’s retirement sparks a competitive NH Senate race
On the Trail: Shaheen’s retirement sparks a competitive NH Senate race
